What do our graduates do after finishing their Harvard Mass. General Med-Peds training?
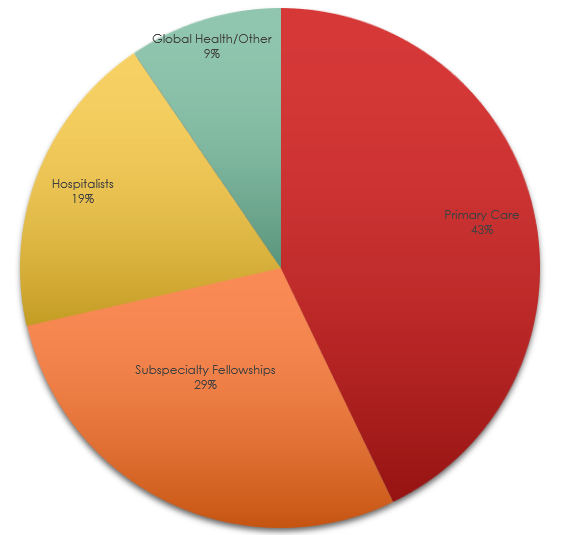
Consistent with national med-peds trends, about 45% of our graduates go into careers in primary care. Approximately 30% choose subspecialty fellowships, 20% work as hospitalists, and 10% in global health respectively. In true med-peds fashion, many of our graduates have careers that span multiple traditional categories (such as working part-time as a hospitalist and part-time in global health, or doing both primary care and advocacy, or working in both academics and industry as an entrepreneur). A more detailed list of our alumni and their career paths is given to applicants during their interview day.
Subspecialties
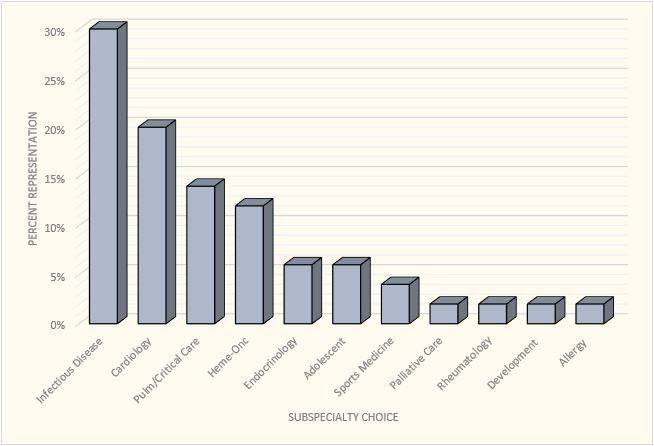
The most popular subspecialty choice for our residents is infectious disease (likely paralleling the high incidence of global health interest), followed by cardiology, heme/onc, critical care, and a variety of other specialties.
For those who do choose fellowships, there is a fairly even distribution between dual fellowships (adult and pediatric), adult training, and pediatric training.
We asked some of our recent graduates to comment on the ways their Harvard Mass. General Med-Peds training prepared them for their careers; their responses are below. You can also view our more extensive list of alumni by clicking here.
Meet Some of Our Alumni
Yamini Krishnamurthy, Class of 2020
After finishing residency at MGH, I moved to New York for an adult cardiology fellowship at Columbia University Irving Medical Center. I’m ultimately interested in pregnancy and cardiovascular disease, pulmonary hypertension, and congenital heart disease, and plan on pursuing a super-fellowship in Adult Congenital Heart Disease after I finish my general cardiology training. I chose to come to MGH because I wanted excellent clinical training in both internal medicine and pediatrics. At MGH, I was fortunate to have excellent mentorship to develop my interest in congenital heart disease and pursue research in this area. Having survived my first year of fellowship, I can safely say that MGH prepared me well for my next step after residency. More importantly, I look back on the friendships that residency brought me, and feel incredibly lucky to be part of the MGH Med-Peds community!
Akash Gupta, Class of 2019
During residency, I was able to use MGH’s amazing resources to explore my varied interests in infectious disease, addiction medicine, and global health. When it came time to decide what to do after graduation, in classic Med-Peds fashion, I figured why not try them all! I am currently an Infectious Disease Fellow at Mass General/Brigham. I had planned to spend my research years of fellowship in South Africa, studying substance use among patients in HIV/TB care programs but COVID-19 unfortunately waylaid those plans. I was able to pivot to other projects, including: Hepatitis C treatment outcomes locally in Boston and a COVID-19 hotel-based shelter program for patients experiencing homelessness and alcohol use disorder near the Navajo Nation. As part of this last effort, I have also been providing volunteer infectious disease care at Gallup Indian Medical Center, part of the Navajo Area Indian Health Service. After fellowship, I will be working as a community-based Infectious Disease provider in the nearby town of Lawrence, a community hard-hit by opiate use disorder and an injection drug use-driven HIV epidemic, and building an integrated ID/addiction program there. The practice also includes another MGH Med/Peds Infectious Disease alum, Dr. John Fangman.
Jing Ren, Class of 2019
I am a generalist, splitting my time between hospitalist work in Boston (both at MGH as well as our community hospital site at Newton Wellesley Hospital) and working for the Indian Health Service in at Northern Navajo Medical Center in Shiprock, New Mexico. While traveling between the two can cause a little bit of whiplash, I love that I still get to see a full spectrum of ages and acuity, inpatient and outpatient. Between my various jobs, I get to do everything from welcoming healthy newborns into the world and doing their first-ever exam, to managing vents/pressors and putting in central lines in the ICU, to helping patients and families make decisions about end of life care. I feel very lucky to have trained in med-peds because of the flexibility it has given me, not only to see patients of any age but also to switch rapidly between different types of services. A lot of med peds training is about learning to adapt quickly to new challenges and using your existing knowledge to help you learn new things. I felt our program really emphasized the development of strong clinical skills and a sense of autonomy starting from an early stage, which has come in handy as a new attending, especially when I am working in rural settings. I came into residency with a strong interest in global health and although I am not currently working abroad, my job now allows me to work closely with underserved populations and in under-resourced settings, while still being plugged into the world of academic medicine. I also love being able to work with residents both on the teaching services here in Boston as well as those doing rotations with IHS, and being able to attend noon conferences and getting to know the current crop of MGH med peds residents when I am in Boston.
Aisha James, Class of 2018
“I loved my training at MGH so much I decided to stay! I am very fortunate to have the opportunity to practice both outpatient and inpatient general medicine & pediatrics, teach trainees, and work to promote health equity at a system level in my current position. My MGH Med-Peds residency provided rigorous clinical training, robust teaching experience, and opportunities for me to develop leadership and advocacy skills through coalition work and mentorship. Most importantly, MGH was a safe and supportive environment where I was able to explore my many interests, and learn from my mistakes and successes.”
Sarah Messmer, Class of 2018
“After finishing residency at MGH, I moved back to Chicago where I now work at the University of Illinois at Chicago (UIC). In my role at UIC, I split my time between internal medicine and pediatrics in both inpatient and outpatient settings. On the adult medicine side, I work in a primary care clinic on the west side of Chicago that focuses on caring for patients living with opioid use disorder. As UIC is a large academic medical center, I have been able to work with many residents and medical students in a variety of clinical settings, and have recently started a role as a House Advisor for the medical school. My training at MGH prepared me to not only provide evidence-based clinical care, but also taught me how to be an effective medical educator. “
Matthew Gartland, Class of 2017
“I am a Med-Peds hospitalist across two hospitals in Boston and the Director of the MGH Asylum Clinic, an organization that provides asylum seekers with forensic medical and psychological evaluations in support of their applications. In residency, I loved the varied clinical and learning environments we worked in. MGH med-peds prepared me with an incredible clinical foundation, skills for leadership, and an amazing network to support my goals. I look around at my role models in residency and the common traits were lifelong learners who demonstrated empathy toward their patients and humility in leadership of their peers. Now three years out of residency, I continue to gravitate to my residency classmates, mentors, and program directors who embody these values for collaboration, challenging clinical problems, or advice on being a physician and raising young children. The MGH Med-Peds community runs deep!”
Rachel Alinsky, Class of 2017
“I’m currently an Assistant Professor in Adolescent Medicine at Johns Hopkins, where I specialize in treating adolescents and young adults with substance use disorders. I became interested in this during Med-Peds residency after seeing many adults on the wards with addiction (most of whom had been struggling with substance use since their teenage years), as well as teenagers and young adults who did not seem to be getting adequate treatment. My Med-Peds training allowed me to see both ends of the spectrum and gain an appreciation for the importance of focusing on early intervention. Thus after residency, I came to Hopkins to pursue a joint fellowship in Adolescent Medicine and Addiction Medicine. In addition to my clinical work seeing youth with substance use disorder, I also perform health services and policy research regarding improving access to addiction treatment for adolescents and young adults.”
Raquel Reyes, Class of 2012
First job after graduation: Uganda Site Director for the MGH Center for Global Primary Care
“I feel privileged to have been a part of the MGH Med-Peds family. I chose a combined residency in Internal Medicine and Pediatrics because of my commitment to serve women and children at home and abroad. In my current position, I attend on the internal medicine and pediatrics wards at a regional referral hospital, and care for adults and children at a level three health center in a small village. Most of the resident physicians I supervise there are Internal Medicine trainees, but most of the patients are children. My Med-Peds training allows me to care for everyone and be able to help other providers care for everyone, too. I chose MGH because I wanted a rigorous clinical training experience. At MGH, I received the kind of training I now need to practice as a competent and confident clinician and clinician educator in a resource-poor setting. Because MGH is so committed to Global Health, not only were there many mentors to provide advice, guidance, and connections, but I was also able to pursue clinical experiences in international settings in each of my final three years of residency. Such clinical experiences helped prepare me for the kind of challenges I now manage in my current role.”
Nina Mayer and Eric Ritchie, both Class of 2012
Working in Chinle, NM, for the Indian Health Service
“Training at MGH gave us the opportunity to be surrounded by amazing colleagues with a variety of experiences and backgrounds, some of whom have worked with Indian Health Services. This allowed us to make contacts with several IHS sites and eventually complete elective rotations on both the Zuni and Navajo Reservations during our residency, which confirmed our interest in providing rural med-peds primary care to the underserved. After graduating, we joined the IHS as medical officers and currently work at the Chinle Comprehensive Health Center in the middle of the Navajo Reservation. Working in Chinle is a very unique experience where we have the opportunity to practice both adult and pediatric inpatient and outpatient care in a resource poor setting. Looking back, our med-peds training, especially at the community hospitals and health centers outside of Boston, helped prepare us for the autonomy that would be required for providing medical care in an extremely remote area.”
Diana Lemly, Class of 2012
Completed an Adolescent Medicine Fellowship at Children’s Hospital Boston
“One of the many things that is so wonderful about the MGH Med-Peds residency is that you are truly prepared to do any fellowship in pediatrics or adult medicine (and even ones that don’t exist yet)! There is a tremendous support to create combined (med-peds) fellowship opportunities or mold existing programs to fit your specific interests. Pretty much anything and everything exists within the Harvard/Partners system and the program helps you make the most use of these resources, even during a busy residency. I decided somewhat late in residency to do a fellowship but had tremendous support from the administration to craft a successful application. It is very special being part of a program that has access to everything, but is still a small, close-knit family.”
Ashley Lamb, Class of 2011
Working in rural North Carolina, practicing primary care at a National Health Service Corps site
“When I arrived in rural North Carolina from MGH I felt like a fish out of water at first, but it didn’t take long for me to realize that I was prepared to do my job as a full-time primary care doctor in a medically underserved area. I have utilized my exposure at MGH to everything from premies to nonagenarians, from the straightforward common cold to rare congenital diseases to develop a great panel of patients who run the gamut. As a med/peds provider, the local pediatricians have been eager to refer their complex patients to me as they age out of pediatrics, and similarly, many adult specialists in the area have referred patients to me who were too complex for the local family physicians and with my MGH experience I have felt comfortable in this role. In addition, at MGH I learned about primary care at a high-quality clinic that used LEAN quality improvement methods and I was able to participate in a community medicine rotation. Both of those experiences helped me feel comfortable helping my office and our community make some tangible improvements since I arrived including setting pediatric standards for the nursing staff (such as weighing babies naked and taking shoes off to measure), establishing and running a Reach Out and Read program, and helping instigate a no-show policy for the clinic. “